Introduction
A Certificate of Need program (CON) limits health care supply unless state health care planners determine a specific “need.” Based on the theory that the economics of health care is unlike any other market, CON laws use central planning to try to reduce health care costs by keeping health care facilities from buying too much equipment, building too much capacity, and adding too many beds. There are a few exemptions to the rule, but in general, medical providers with plans to build or expand an existing health care facility, offer new services, or update major medical equipment, must ask for, and receive, permission from the State Health Coordinating Council (SHCC).
Intending to cut down on health care cost inflation, Congress enacted CON laws under the federal Health Planning Resources Development Act in 1974. However, the federal government repealed the CON mandate in 1987 because the program did not effectively restrain costs. In fact, four decades’ worth of data and research into CON laws consistently finds that such laws fail to lower health care costs. On the contrary, limiting the supply of health services is far more likely to increase health care costs because doing so reduces competition as well as access to care.
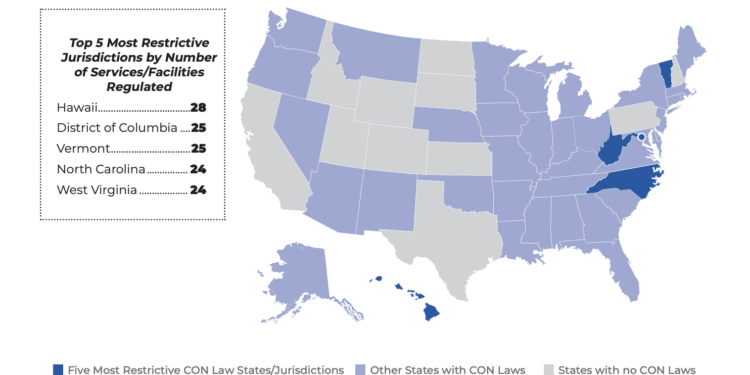
Since the federal CON repeal, 15 states have scrapped their CON programs. North Carolina has not. The state still has one of the most stringent CON programs in the nation, regulating 24 services that range from kidney dialysis units to hospital beds and rural ambulatory surgical centers.
Some minor CON rollbacks have been implemented over the years. For instance, a 2005 law allowed gastroenterologists to perform colonoscopies in their own endoscopy units. This increased access to service and lowered prices. More recently, the state legislature allowed select rural hospitals to bypass the CON process when adding or converting unused acute-care beds into inpatient behavioral-health beds.
Furthermore, as part of legislation passed in 2023 to expand Medicaid, some additional CON restrictions were rolled back. These included: urban ambulatory surgical centers in counties with populations above 125,000, MRI scanners in urban counties, diagnostic equipment if the total investment is less than $3 million, psychiatric beds and chemical-dependency treatment beds, and licensed home-care agencies providing early and periodic screening, diagnosis, and treatment services (EPSTD) to children up to 21 years of age.
The degree to which CON laws restrict the efficient and effective provision of medical care was on full display during the COVID-19 pandemic. As state hospitals and health care providers geared up to treat the influx of seriously ill patients, Gov. Roy Cooper suspended the complete CON process. In its place, the state used a more expedited method to approve increases in bed capacity or the movement of medical imaging equipment. This illustrates the ineffectiveness of CON laws. Only by suspending those laws could priceless resources be made available to COVID patients. The lesson learned during the pandemic applies even in regular times. Providers on the ground are far better equipped than a bureaucratic board in Raleigh to make determinations of health care needs.
Ideally, all hospitals and health centers, not the state, should be able to decide for themselves how to provide resources. Fully eliminating all CON review requirements would result in a significant victory for patients.
Key Facts
When CON laws were implemented, policymakers hoped to tackle massive health care inflation due to the “cost-plus” reimbursement method under which providers were paid at the time. However, years of research have shown that despite the presence of CON laws in most states, health care costs continued to rise, and the federal government realized these laws failed to achieve the goal of keeping inflation in check.
The impact of CON laws extends beyond artificially higher prices. North Carolina’s CON program reduces access to health care for local communities and consumers, especially those who live in small towns and rural areas. States with CON laws have 30% fewer rural hospitals and 13% fewer rural ambulatory surgical centers than states without CON laws. The elderly, the poor, people under time constraints, and people with emergency medical needs would be better served by having medical services nearby, rather than traveling to a hospital or clinic fortunate enough to have received CON approval for a service or procedure.
Supporters of CON laws claim that such programs are necessary to ensure hospitals can provide “charity care” or accommodate those without insurance or those who have trouble paying for medical care. However, studies have shown there is no difference in the amount of charity care between states that impose CON laws and states that do not.
Growing mental health and substance abuse problems in North Carolina are exacerbated by CON laws. A 2021 study found that if the state scrapped its CON laws, it would likely have an additional three psychiatric hospitals. The study also estimates that in a CON-free North Carolina, six additional substance-abuse facilities would accept private insurance, and 12 more would accept Medicaid.
Recommendations
1. Fully Repeal Certificate of Need.
CON laws restrict access to care, put government control ahead of patients and doctors, handcuff health providers from offering care in their communities, increase health care costs by preventing competition, undermine the doctor/patient relationship, and add anxiety about the quality of care when people are most vulnerable. North Carolina families deserve access to quality care and lower costs, unencumbered by government control.
Services That Require a Certificate of Need in North Carolina
- Air Ambulance
- Ambulatory Surgery Centers (ASCs) in rural counties
- Assisted Living & Residential Care Facilities
- Burn Care
- Cardiac Catheterization
- Computed Tomography (CT) Scanners
- Gamma Knives
- Home Health
- Hospice
- Hospital Beds
- Intermediate Care Facilities (ICFs) for Individuals with Intellectual Disabilities
- Linear Accelerator Radiology
- Lithotripsy
- Magnetic Resonance Imaging (MRI) Scanners) in rural counties
- Mobile Hi Technology (CT/MRI/PET, etc.)
- Neonatal Intensive Care
- New Hospitals or Hospital-Sized Investments
- Nursing Home Beds/Long-Term Care Beds
- Open-Heart Surgery
- Organ Transplants
- Positron Emmission Tomography (PET) Scanners
- Radiation Therapy
- Rehabilitation
- Renal Failure/Dialysis
Jurisdictions With the Most Restrictive Certificate-of-Need Laws
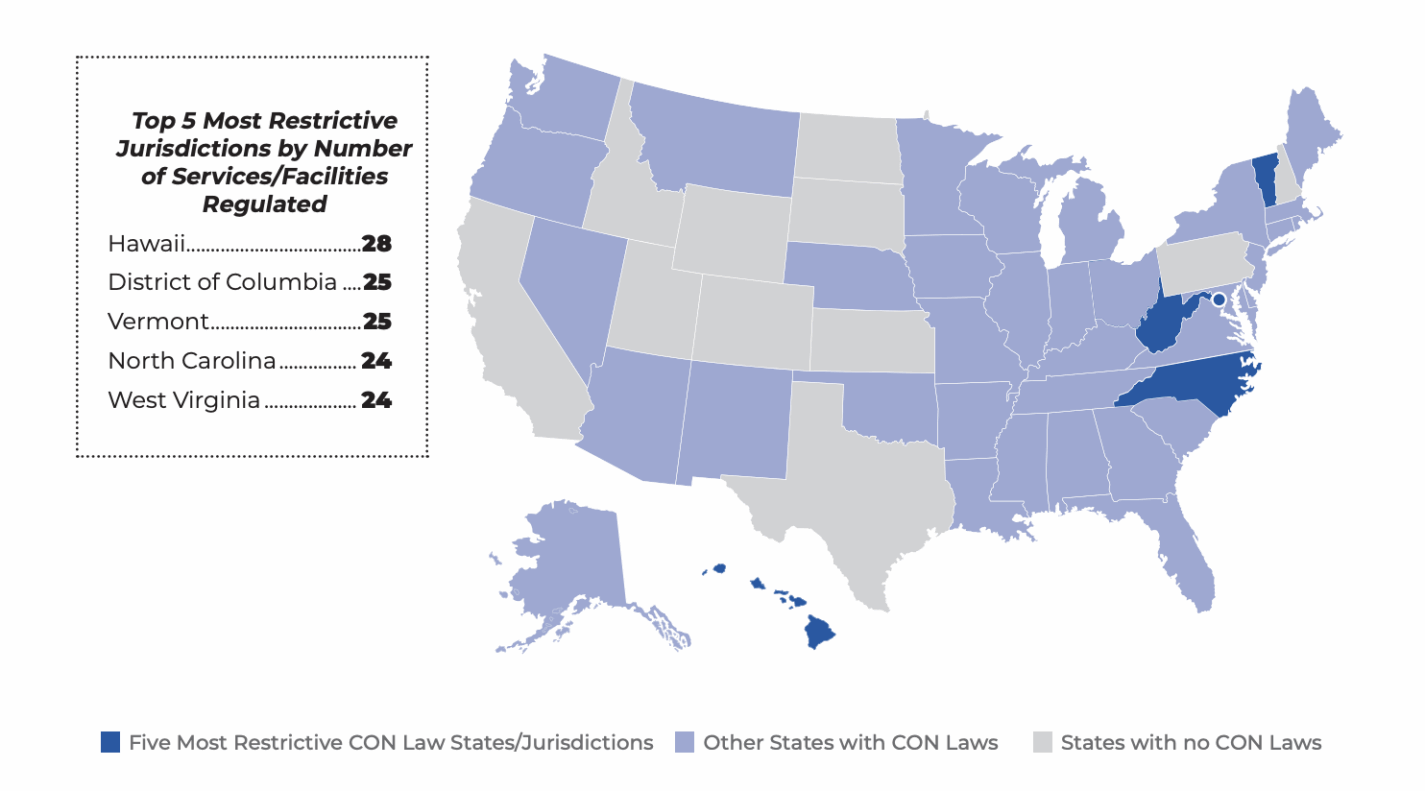
Source: Mercatus Center