- Surging Medicaid expansion enrollment is crowding out the state’s most vulnerable
- North Carolina has the slowest median emergency room visit time in the Southeast
- The One Big Beautiful Bill Act is set to dismantle Medicaid expansion’s funding model
When Medicaid was established in 1965, it was not a sweeping guarantee of health care for all; it was a narrow commitment aimed at serving society’s most vulnerable: the disabled, the blind, the elderly, foster children, and single-parent families with incomes well below the federal poverty level.
Over time, policymakers broadened that commitment to include two-parent households and children in families earning up to 211 percent of the federal poverty level — a stretch, but one that remained tethered to the original intent of protecting those least able to care for themselves.
The decision to extend Medicaid coverage to childless, able-bodied adults through expansion, however, is not a continuation of that moral vision, it is a distortion of it. The expansion actively harms the truly vulnerable by diverting limited resources, funding, and provider capacity away from the disabled, the blind, the elderly, and impoverished children who depend on Medicaid as a lifeline.
Now is the time to repeal Medicaid expansion. The federal “One Big Beautiful Bill Act” is poised to dismantle the state’s Medicaid expansion financing model. Policymakers face a clear choice: Either raise taxes to prop up a program that diverts resources to able-bodied adults or end expansion before it threatens care for the genuinely marginalized.
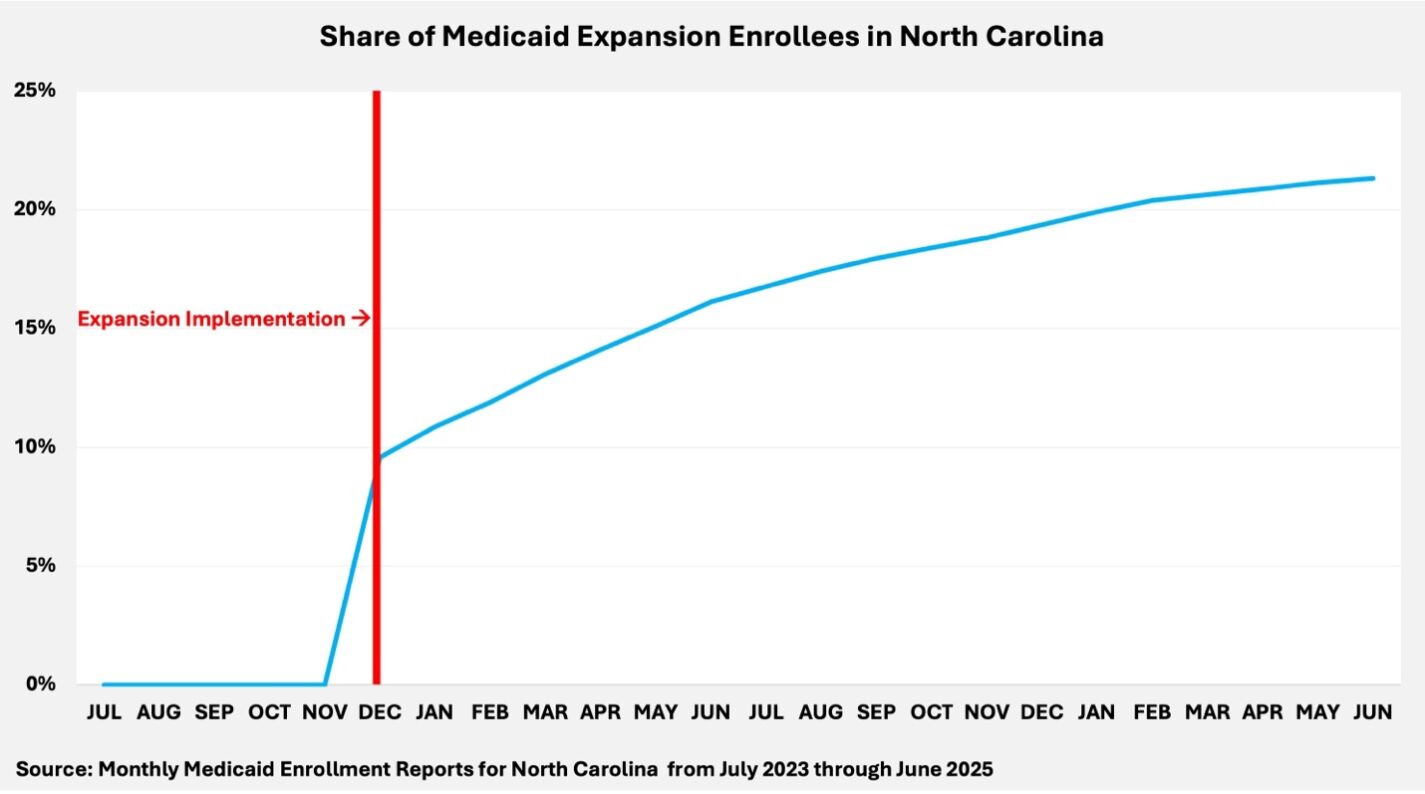
In the short span of 19 months since expansion, expansion enrollees have jumped from accounting for 0 percent of Medicaid enrollees to 21.3 percent.
Medicaid enrollment trends
Since Medicaid expansion took effect in December 2023, nearly 670,000 able-bodied adults have enrolled in the program, despite initial estimates that enrollment would not reach 600,000 until December 2025. This surge in enrollment has strained the Medicaid program’s capacity. In the short span of 19 months since expansion, expansion enrollees have jumped from accounting for 0 percent of Medicaid enrollees to 21.3 percent.
The rapid addition of nearly 700,000 new enrollees has led to a reallocation of resources that, in practice, crowds out traditional Medicaid populations, such as the disabled, the blind, the elderly, and low-income children.
For example, from November 2023 through June 2025, the share of aged, disabled, or blind Medicaid enrollees in North Carolina dropped from 16.2 percent to 14.4 percent. This decline underscores how the influx of able-bodied adults under expansion has diluted the program’s focus, shrinking the proportional representation of those with the most significant medical needs.
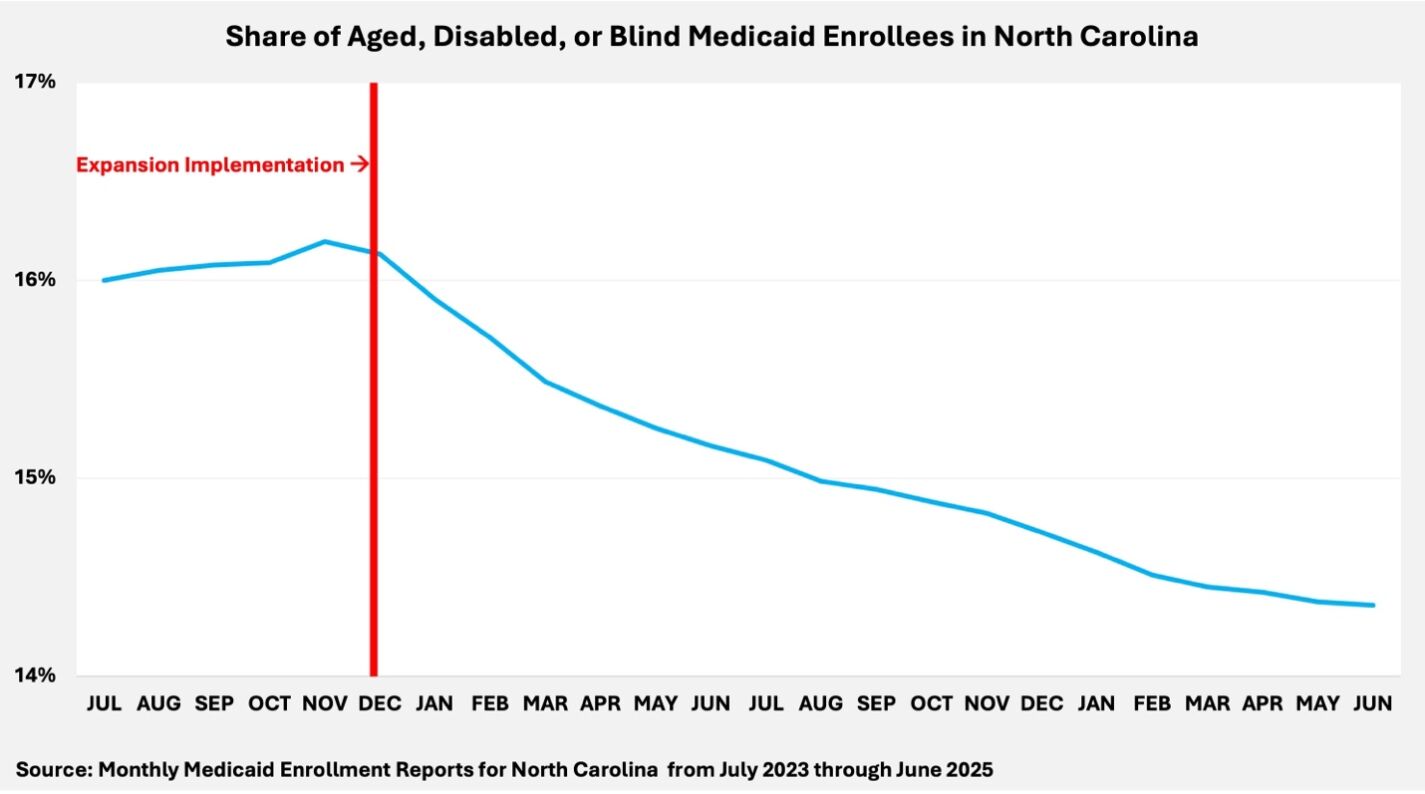
Likewise, the share of children from needy families or in foster care has declined from 19.1 percent to 17.3 percent. This shift reflects how expansion has altered the internal composition of Medicaid, drawing attention and administrative priority away from vulnerable children. As healthy adult populations absorb more resources, the children the program was initially designed to protect are becoming a smaller share of its focus.
 Emergency room delays
Emergency room delays
North Carolina’s health care system has become increasingly strained due to Medicaid expansion. While some argue that we have more than enough resources to accommodate traditional Medicaid recipients and the new expansion population, the data tell a different story.
Even before expansion, North Carolina ranked among the worst in the nation for emergency room efficiency, with a median visit time of 2 hours and 36 minutes in fiscal year (FY) 2019, placing the state 11th slowest. By FY 2024, that time had stretched to 3 hours and 15 minutes, dropping North Carolina’s standing to 7th slowest nationwide and the slowest in the Southeast.
Rather than alleviating pressure on emergency rooms, Medicaid expansion flooded an already overburdened system with hundreds of thousands of new enrollees, lengthening delays and stretching hospital capacity even thinner.
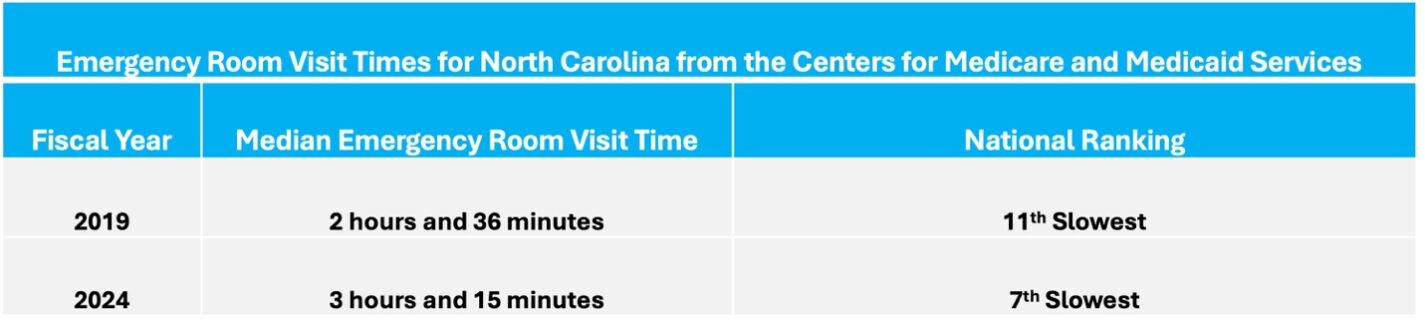
North Carolina has also seen a 50 percent increase in the share of emergency room patients who leave without treatment. In practical terms, for every 100 people who walked into an emergency room in FY 2019, two left before receiving care. By FY 2024, that number had grown to three out of every 100 patients. That may sound small, but it represents tens of thousands of North Carolinians who showed up to the emergency room in pain only to leave without being cared for.
Closing thoughts
The promise of Medicaid was to care for the truly vulnerable, not to cover able-bodied adults. But that promise is unraveling. Since expansion, emergency room visit times in North Carolina have climbed to over three hours, the slowest in the Southeast, while more patients leave without ever being seen.
Meanwhile, the One Big Beautiful Bill Act threatens the funding model that props up expansion, forcing policymakers to raise other taxes to sustain an overcrowded system or repeal expansion to restore Medicaid’s original mission. The clock is ticking — and the most vulnerable cannot afford to be kept waiting.











